

|
Clinical Cases |
|
Hip Replacement
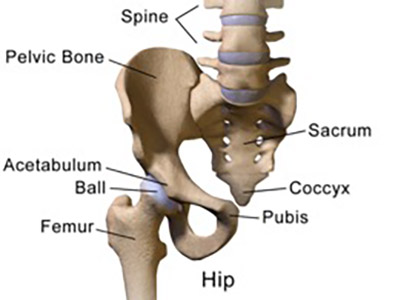
Arthroplasty is defined as the surgical reconstruction or replacement of a joint. Hip arthroplasty (commonly known as hip replacement) is a surgical procedure that is done to fully or partially replace a hip joint that has become malformed, dysfunctional, and/ or painful as a result of arthritis, trauma, congenital defect, or bone malignancy. The most common indication for hip replacement is osteoarthritic pain that has become unmanageable by medication or physical therapy.
Anatomical Considerations of Different Surgical Approaches to Hip Replacement
The many different surgical approaches to total hip replacement have many steps in common. These steps are typically those that come after the hip joint has been visualized and dislocated to expose the femoral head and acetabulum. Once the femoral head is exposed it is removed and the femur is prepared for implantation of the femoral stem, which will hold the prosthetic head of the femur. The acetabulum is then reshaped and prepared for insertion of the prosthetic cup implant. Once all of the prostheses are in place the joint is put back together and tested for fit and range of motion. If the surgeon is pleased with the results, muscles are reattached and incisions sutured close.
Procedural variability in the total hip arthroplasty comes in the approach to visualization of the hip joint. These approaches are all named based on their anatomical position in reference to the gluteus medius muscle. We will discuss 4 of these approaches:
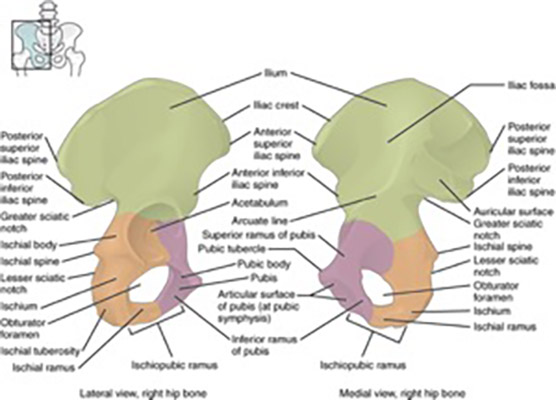
- Anterior Approach - This approach takes advantage of the internervous plane that exists superficially between the sartorius and tensor fascia latae (between the femoral and superior gluteal nn., respectively), and deeply between the rectus femoris and gluteus medius (also between femoral and superior gluteal nn., respectively). An incision is made from the middle of the iliac crest to the anterior superior iliac spine, and then curved distally and laterally to a point below the lesser trochanter. The lateral femoral cutaneous nerve, which passes beneath the inguinal ligament and over the sartorius near the anterior superior iliac spine, must be carefully avoided when making this incision. The gluteus medius and tensor fascia latae are then detached from their origin on the ilium. Dissection then begins through the deep fascia to visualize the tensor fascia latae laterally and the rectus femoris medially. The ascending branch of the lateral circumflex femoral artery should be visible between the rectus femoris and tensor fascia latae, and is ligated after visualization to help maintain hemostasis during the procedure. The anterior capsule of the hip joint can be visualized after opening the plane between the rectus femoris and the tensor fascia latae. The capsule is then cut open to visualize the femoral head, which is then dislocated from the acetabulum. At this point the joint is exposed, and the surgeons work on replacing the damaged joint with a prosthetic one.
- Anterolateral Approach - In this approach the surgeon uses the interval between the tensor fascia latae and the gluteus medius to gain access to the femoral neck and hip joint. A skin incision is started a couple of cm posterior to the anterior superior iliac spine. The incision first moves posterior and distally, and then once it is in line with the shaft of the femur it curves to follow the femur distally. The incision is opened and the interval between the tensor fascia latae and the gluteus medius is identified. This interval is developed proximally by blunt dissection in order to protect the inferior branch of the superior gluteal nerve (which innervates tensor fascia latae). The tensor fascia latae is retracted anteriorly and gluteus medius is retracted posteriorly to expose the joint capsule. Sometimes the vastus lateralis must be reflected proximally 1-2 cm as well to expose the femoral head. The joint capsule is then cut to expose the femoral head, and the joint is dislocated by external rotation.
- Direct Lateral Approach - An incision is made from 5 cm proximal to the greater trochanter to 5 cm distal to it. The tensor fascia latae is then incised in line with the skin incision to expose the gluteus maximus. The gluteus maximus is now divided along its aponeurosis to expose the greater trochanter (care must be taken here to protect the sciatic nerve). The gluteus medius is seen attaching proximally and the vastus lateralis attaching distally t the greater trochanter. Both muscles are incised longitudinally over the greater trochanter and the anterior portions of the muscle are separated from their insertion sites. This exposes the gluteus minimus tendon, which is then detached from its insertion on the greater trochanter. The capsule is now exposed and ready to be opened for the hip replacement.
- Posterolateral Approach - The most commonly used approach due to its avoidance of hip abductors and its technical simplicity. Skin incision is made longitudinally with one-third the length above the greater trochanter, one-third below the greater trochanter, and the final part curving above the greater trochanter in the direction of the gluteus maximus fibers. The tensor fascia latae and deep gluteal fascia are incised in line with the skin incision, and the gluteus maximus is bluntly dissected to expose the posterior border of gluteus medius. The posterior border of gluteus medius is then retracted. The piriformis, superior and inferior gemelli, quadratus femoris, and the obturator internus are then tagged and released from their insertions. These muscles can then be pulled posteriorly to act as a protective sling for the sciatic nerve. Finally, the gluteus minimus must be separated from the capsule to expose the hip joint and femoral head.
Hip Replacement on Plain Film and CT Scan
The image below is the scout film of cadaver 33487. Notice that the left hip joint has been replaced with a prosthetic joint consisting of a femoral stem attached to a ball that sits inside a prosthetic cup.
