

|
|
||||||||||||
Dissector Answers - Stomach, Spleen, Duodenum, & Pancreas |
|||||||||||||
Learning Objectives:
Upon completion of this session, the student will be able to:
- Identify the parts of the stomach and describe its spatial relationships to surrounding organs and mesenteries.
- Describe the blood supply of the abdominal foregut via branches of the celiac artery, and the basic pattern of lymphatic drainage in this region.
- Describe the anatomy of the foregut peritoneal ligaments, omenta and omental bursa, and their development from the embryological ventral and dorsal mesogastria.
- Describe the pattern of parasympathetic innervation of the GI tract.
- Identify and describe the parts and peritoneal relationships of the duodenum and pancreas.
- Describe the pattern of common vasculature of the duodenum and pancreas.
- Trace the potential collateral blood flow between celiac and superior mesenteric arterial territories, and between superior and inferior mesenteric arterial territories.
- Trace the pathway of common entry of the bile ducts and pancreatic ducts into the 2nd part of the duodenum.
Learning Objectives and Explanations:
1. Identify the parts of the stomach and describe its spatial relationships to surrounding organs and mesenteries. (W&B 448-450, N 260,264,265,267 or TG 5-01,5-18A, 5-18B)Parts:2. Describe the blood supply of the abdominal foregut via branches of the celiac artery, and the basic pattern of lymphatic drainage in this region. (W&B 451-456, N 258,290,291,292,304,307 or TG 5-19,5-27,5-35A,5-35B, TG5-37)Curvatures:
- cardia: immediately surrounding the esophageal opening
- fundus: the part that extends to the left and superior to the esophageal opening, filling the dome of the diaphragm. It is separated from the esophageal opening by the cardiac notch. (Latin, fundus = bottom, base)
- body: between the fundus and the pyloric portion
- pyloric portion (pylorus): includes the pyloric antrum (the entryway to the pyloric canal), the pyloric canal, and the pylorus proper, which thickens to form the pyloric sphincter. It is separated from the body by the angular notch. (Greek, pyloros = gatekeeper, Latin, antrum = cave)
Orientation and relationships:
- lesser curvature: forms the right/superior/concave border of the stomach
- greater curvature: forms the left/inferior/convex border of the stomach
The plane of the stomach is oblique, running from the fundus to the pylorus inferiorly, ventrally, and to the right. It has, then, effectively an anterior and a posterior surface. The left anterior surface contacts the diaphragm and the abdominal wall, while on the right side the anterior surface lies against the liver. The posterior surface of the stomach forms the anterior wall of the omental bursa. The stomach is almost entirely covered in peritoneum, except where vessels run along the curvatures and where the peritoneum reflects to form ligaments, or attachments to other viscera. These include the hepatogastric ligament from the lesser omentum, and the gastrophrenic, gastrosplenic, and gastrocolic ligaments from the greater omentum.
3. Describe the anatomy of the foregut peritoneal ligaments, omenta, and omental bursa. Describe their development from the embryological ventral and dorsal mesogastria. (W&B 436-443, N 261,264,267,279 or TG 5-12,5-18A,5-18B,5-21, Learning Module)
There are three branches of the celiac trunk:
- left gastric artery: supplies the lesser curvature of the stomach, anastomoses with the right gastric artery
- splenic artery: supplies the spleen. It gives off left gastro-omental artery, which supplies the greater curvature of the stomach and anastomoses with the right gastro-omental artery.
- common hepatic artery: supplies the liver via the proper hepatic artery. The latter gives off the right gastric artery, which supplies the lesser curvature of the stomach and anastomoses with the left gastric artery. The common hepatic also gives off the gastroduodenal artery, which supplies the duodenum, pancreas, and, via the right gastro-omental artery, supplies the greater curvature of the stomach.
Looking at things the other way around, the stomach is supplied by:
- right gastric artery: a branch of the proper hepatic artery, from the common hepatic artery, which is a primary branch of the celiac trunk
- left gastric artery: a primary branch of the celiac trunk
- right gastro-omental artery: a branch of the gastroduodenal artery, which is a branch of the common hepatic artery, which is a primary branch of the celiac trunk (Latin, duodeni = 12 each (the duodenum is about 12 finger breadths long))
- left gastro-omental artery: a branch of the splenic artery, which is a primary branch of the celiac trunk
The lymphatic drainage of the stomach is a bit complex. Lymph from the stomach goes towards one or the other of the curvatures, draining to four main areas:
Towards lesser curvature:Towards greater curvature:
- left gastric nodes: afferents to these drain a large portion of the stomach. Efferents from here follow the left gastric blood vessels and go to the celiac nodes.
- right gastric nodes: drain a small portion of the pylorus. Efferents go to hepatic nodes, eventually dumping into celiac nodes.
- pancreaticosplenic nodes: drain the spleen, pancreas, and the left fundus and body of the stomach. They send lymph to the celiac nodes.
- right gastro-omental nodes: drain the body and pyloric portion of the stomach. Efferents go from here to the pyloric nodes, then the hepatic nodes, and finally the celiac nodes.
In a nutshell, lymph goes toward one of the curvatures and eventually ends up in the celiac nodes. There are no "left gastro-omental nodes".
4. Describe the pattern of parasympathetic innervation of the GI tract. (W&B 456-457 (stomach), 465-466 (duodenum), 482 (SI), 488 (LI), N 228,309,310,311,314B or TG 8-17, TG8-21)It is logical here to consider the development first. Initially the entire primordial gut tube is suspended in the center of the abdominal cavity by a "dorsal common mesentery", which is attached to the midline of the posterior body wall. As development progresses, a portion of the tube begins to enlarge into a stomach. From this point on, the attachments of the stomach to the body wall are called the ventral mesogastrium (ventral mesentery) and the dorsal mesogastrium (dorsal mesentery). The spleen and dorsal pancreas develop in the dorsal mesogastrium. Therefore, structures involving the spleen and the posterior part of the developing stomach (which becomes left and inferior), are derived from the dorsal mesogastrium. These include:
- greater omentum:
- gastrophrenic ligament (Latin, ligare = band, tie)
- gastrosplenic ligament
- gastrocolic ligament (with the omental apron hanging from it)
- splenorenal ligament
The liver begins to develop in the ventral mesogastrium, so structures involving the liver and its attachment to both the stomach and the body wall come from the ventral mesogastrium. These include:
- lesser omentum:
- hepatogastric ligament
- hepatoduodenal ligament
- ligaments of the liver:
- falciform ligament
- coronary ligament
- right and left triangular ligaments
Now we can think about the anatomy. (Come on... I know you want to!) As you've probably figured out by now, the relationships of the abdominal viscera can be very confusing as a result of that whole umbilical herniation and 270-degree rotation during development. Remember the descriptions of how things started, with the gut tube attached to the gut wall via the primitive mesentery. From there, the final relationships are only a gut rotation away.
Greater omentum: This started as a connection between the posterior stomach and the posterior abdominal wall. The stomach rotates such that what was the posterior surface becomes more left and inferior. Part of this original connection remains as the gastrophrenic ligament. Furthermore, by now the colon has done all of its business and the transverse colon is sitting there, right underneath the stomach, and has its own attachment to the posterior abdominal wall. The greater omentum grows a great deal, becoming the big "abdominal policeman" (omental apron) that we all know and love. "But, how does the stomach end up connected to the transverse colon via the gastrocolic ligament?" you ask. The greater omentum ends up draped over the transverse colon and the transverse mesocolon, and ends up fusing with both. This fusion effectively creates the gastrocolic ligament by connecting the stomach to the transverse colon. (See #5 below.) The spleen develops within the dorsal mesogastrium, between the stomach and the body wall. The tissue between the stomach and the spleen remains as the gastrosplenic ligament.
Lesser omentum: It started as the connection between the anterior stomach and the anterior body wall. As the stomach rotates, what was anterior becomes right and superior. At the same time, the liver is developing between the stomach and the body wall, within this ventral section of peritoneum. The liver ends up being huge, so when all is said and done, all of the former connection between the stomach and the ventral body wall is connection between the stomach (including part of the duodenum) and the liver, the hepatogastric and hepatoduodenal ligaments. All of the rest of the tissue, that is, what was between the liver and the body wall, ends up as the ligaments of the liver: the falciform, coronary, right triangular, and left triangular ligaments.
To get a good idea of what is going on with all of the "twisting around", check out the several gut rotation movies in Animations.
5. Identify and describe the parts and peritoneal relationships of the duodenum and pancreas. (W&B 458-466, N268, N278, N279, TG5-26,TG5-01,TG5-26)Parasympathetic innervation to most of the GI tract, from the stomach to the splenic flexure of the colon, is originally from the vagus nerves (CN X). Along the way they will form various plexuses and then reorganize into nerves, but it is all vagus derived. (For example, after the esophageal plexus, fibers come back together to form the anterior and posterior vagal trunks, which supply the stomach and other viscera.) For the portions of the colon distal to the splenic flexure, the parasympathetic innervation is from S2-S4, via the pelvic splanchnic nerves and the inferior hypogastric plexus. (Recall that arterial blood supply to the colon also had a "transition" at the splenic flexure.)
6. Describe the pattern of common vasculature of the duodenum and pancreas. (W&B 463-465, N301,N302,N304, TG5-27B,TG5-27C)Because of their close functional and spatial relationships, as well as a shared blood supply, it is logical to consider the duodenum and the pancreas together.
The duodenum (Latin, duodeni = 12 each) (N268, TG5-01) is the connecting pipe between the stomach and the small intestine. (FYI: both "du-uh-DEE-num" and "du-AH-de-num" are correct pronunciations.) It is mostly retroperitoneal. The exceptions are the first 2cm of the first part (ampulla, duodenal cap) and the duodenojejunal junction. (The latter is not technically part of the duodenum.) The duodenum has four parts: (N278, N279, TG5-26B.TG5-26C)
- superior (1st): horizontal, lies at L1 level. This part is:
- posterior to the gallbladder and quadrate lobe of the liver;
- anterior to the bile duct, the gastroduodenal artery, the portal vein, and the IVC;
- inferior to the neck of the gallbladder; and
- superior to the neck of the pancreas.
- descending (2nd): vertical, descends from L1 to L3, point of entry for bile and pancreatic ducts. This part is:
- posterior to the transverse colon and mesocolon, and also posterior to part of the jejunum;
- anterior to the hilum of the right kidney, the renal vessels, the right ureter, and the right psoas major muscle; and
- lateral to the head of the pancreas and pancreatic and bile ducts.
- horizontal (3rd): horizontal, crosses L3 vertebra. This part is:
- posterior to the SMA, SMV, and parts of the jejunum;
- anterior to the right psoas major muscle, the IVC, the abdominal aorta, and the right ureter; and
- inferior to the head of the pancreas (on the right side) and the SMA and SMV.
- ascending (4th): vertical, ascends from L3 to L2. This part is:
- posterior to the root of the mesentery, parts of the jejunum;
- anterior to the left psoas muscle;
- lateral to the head of the pancreas (on the left side); and
- inferior to the body of the pancreas.
For the opposite viewpoint of the above list, from the duodenum's "perspective", see N298 or TG5-26.
The pancreas (Greek, pankreas = sweetbread) is an accessory digestive organ. It is retroperitoneal, except for its tail. It makes enzymes that aid in chemical digestion of food. (This is its "exocrine" role. The pancreas also has an "endocrine" role with insulin, glucagon, and all that business.) It is also divided into four parts:
- head: attached to the duodenum, includes the uncinate process. The head of the pancreas rests on the IVC, the right renal artery and vein, and the left renal vein.
- neck: short junction between the head and the body. It overlies the SMA and SMV, including the junction of the SMV and splenic vein to form the portal vein. It is posterior to the pylorus of the stomach.
- body: between the neck and the tail. Posteriorly it contacts the SMA, abdominal aorta, and the left suprarenal (adrenal) gland, kidney, and renal vessels. Anterior to it is the omenental bursa.
- tail: the somewhat mobile end of the pancreas. It lies within the splenorenal ligament and contacts the left kidney, left colic (splenic) flexure, and the hilum of the spleen posteriorly.
7. Trace the potential collateral blood flow between celiac and superior mesenteric arterial territories, and between superior and inferior mesenteric arterial territories. (W&B 463-465, 487, N301,N302,N304,N305,N306,TG5-13,TG5-14,TG5-27B,TG5-27C)Both the duodenum and the pancreas receive blood from the celiac trunk and the superior mesenteric artery. They serve as a site for anastomosis between these two large systems. The body and tail of the pancreas are supplied mostly by branches of the splenic artery, namely the great, superior, caudal, and dorsal pancreatic arteries.
8. Trace the pathway of common entry of the bile ducts and pancreatic ducts into the 2nd part of the duodenum. (W&B 461, 470-472, N294,N298,N297,TG5-24B,TG5-24C,TG5-26)As described above, there is collateral circulation between the celiac and superior mesenteric arterial territories as they both supply the head of the pancreas and the duodenum. Collateral circulation between the superior mesenteric and inferior mesenteric arterial territories occurs via the marginal artery, which is effectively a very large arterial arch that supplies the entire colon (not discussed in Moore).
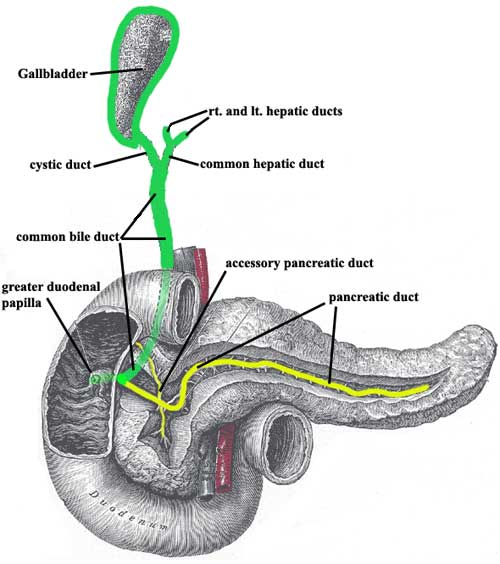
This image is not to scale with regard to the size of the gallbladder relative to the other organs. Connectivity is also not anatomically accurate, but is meant to be illustrative.
Fresh bile from the liver drains out via the right and left hepatic ducts, which join to become the common hepatic duct. Stored bile leaves the gall bladder via the cystic duct. (Please note that bile from the liver also enters the gallbladder via the cystic duct, by traveling retrograde, when the GI tract does not need bile to aid in digestion of food and bile is therefore stored.) The common hepatic duct joins the cystic duct to form the common bile duct. (Greek, kystis = bladder, pouch)
The main pancreatic duct begins in the tail of the pancreas and receives tributaries all along its path to the head of the pancreas. Often there is also a separate accessory pancreatic duct (N 298), which drains independently into the duodenum via the lesser (minor) duodenal papilla.
Usually, the main pancreatic joins the common bile duct right before entering the duodenum, so they both dump their contents via the greater (major) duodenal papilla (comprised of the ampulla of Vater, or hepatopancreatic ampulla, and the sphincter of Oddi). There is variation in this anatomy, for example, independent dumping of the pancreatic and common bile ducts into the duodenum via separate papillae (N N297).
Cultural enrichment: Check out these sections from the 1918 version of Gray's Anatomy of the Human Body! Some of the terms are (of course) out-of-date, but the illustrations are timeless.
The Stomach - The Spleen - The Abdominal Aorta - Surface Anatomy of the Abdomen -Surface Markings of the Abdomen
Questions and Answers:
1a. Examine how the greater omentum has combined with and assists in the formation of the transverse mesocolon. (N 261,263,264, TG 5-12,5-18)2a. Define the omental bursa (lesser sac). How does it develop? What is its entrance? What are its boundaries? (N 264,265,335,336, TG 5-18,5-42)"The layers [of the omental apron] returning from the fold to the body wall lie against the transverse colon and the superior layer of its mesocolon, and these opposed parts fuse. Thus, the inferior extension of the greater omentum becomes the gastrocolic ligament and helps form the transverse mesocolon."
3a. Follow along the proper hepatic artery into the hepatoduodenal ligament until you locate the right gastric artery. Trace it to the lesser curvature of the stomach. Does it anastomose with the left gastric artery? (N 290, TG 5-19)The omental bursa is a space that exists between the stomach and the posterior wall of the abdominal cavity. It gives the stomach room to expand after a meal. It is created by the rotation of the stomach during development so that the greater curvature faces left (and inferiorly) and the lesser curvature faces right (and superiorly). The growth of the liver helps to define the borders of the omental bursa. Your fingers can be stuck into the space through the omental foramen. The boundaries of the omental bursa are as follows:
- superior: caudate lobe of liver
- ventral: the stomach
- posteriorly: posterior abdominal wall
- inferior: the duodenum
4a. Does the left gastro-omental artery anastomose with the right? (N 290, TG 5-19)Yes, the right gastric anastomoses with the left.
5a. How does the splenic artery reach the spleen? How do its branches reach the stomach? (Note relations to stomach, kidney and left colic (splenic) flexure.) (N 291, TG 5-19)You bet.
6a. What is the coronary vein? (N 299, 302, TG 5-19, 5-28)The course of the splenic artery from the celiac trunk to the spleen is very tortuous. Along the way, it is partially embedded in the superior part of the pancreas, and therefore more or less runs in the floor of the omental bursa. It passes through the splenorenal ligament, dividing into several branches to supply the spleen. Near its end, the splenic artery gives off the left gastro-omental artery, which supplies the greater curvature of the stomach and anastomoses with the right gastro-omental artery. It also gives off four or five short gastric branches, which supply some blood to the fundus of the stomach. They anastomose with both the left gastric and the left gastro-omental arteries.
7a. Organize the lymph drainage of the stomach and spleen. (N 258, 304, 307, TG 5-37, 5-35, 5-35)The coronary vein is the circular venous structure formed by the anastomoses of the right and left gastric veins. Its circular course along the lesser curvature is said to crown the stomach, hence its name.
8a. Look for a hepatic branch of the anterior vagal trunk passing within the lesser omentum to the liver and then to the duodenum. Do you have an accompanying hepatic branch of the left gastric artery? (N 309, 310)See #2 above.
9a. Consider distribution and function of the vagus nerve. (N 228, 309, 310, 311, TG 4-37)The anterior vagal trunk sends branches to the stomach and liver, usually with an extension of this hepatic branch going down to the duodenum. The posterior vagal trunk also branches to stomach, but has no hepatic branch. It also branches to the celiac ganglion.
10a. How do sympathetic branches distribute to the stomach? (N 205, 310, 311, TG 4-38)See #4 above.
11a. Organize the mesenteries of the stomach, considering their contents and functional importance to the stomach. (N 261, 264, 267, TG 5-12, 5-18, 5-18)Well, if you stumble across a ferocious bear, your stomach should take a break. This allows energy and oxygen to be used for that panic-induced sprint you are about to undertake. So, sympathetic innervation is essential. It is provided from T5-T9 via the greater thoracic splanchnic nerve, to the celiac ganglion and plexus.
12a. Is the superior (1st) part of the duodenum peritoneal or retroperitoneal? (N275,N278,TG5-18,TG5-26)See #3 above.
13a. What is the suspensory muscle of the duodenum? ( N270,TG5-26)Both. The first 2 cm has a mesentery, the hepatoduodenal ligament. The rest of the superior part of the duodenum is retroperitoneal.
14a. What is the relation of the horizontal (3rd) part of the duodenum to the superior and inferior mesenteric arteries? (N278,TG5-26)The suspensory muscle of the duodenum (also known as the ligament of Trietz) is a thin sheet of muscle fibers derived from the right crus of the diaphragm that suspends the fourth part of the duodenum (the duodenojejunal flexure or junction) from the posterior abdominal wall.
15a. Carefully trace the common bile duct as it courses behind the first part of the duodenum and the head of the pancreas to the medial wall of the second part of the duodenum. Does an artery cross it? (N304,TG5-27)The 3rd part of the duodenum is crossed anteriorly by the SMA and vein. It is superior to the IMA.
16a. How does the posterior arcade differ from the anterior arcade? (N301,N302,N304,TG5-27B,TG5-27C)The posterior superior pancreaticoduodenal artery from the gastroduodenal artery passes anterior to the duct as it passes to the right, then travels inferiorly posterior to the common bile duct.
17a. Do you find veins with the arterial arcades of the pancreas and duodenum? (N301,N302,N304,TG5-27BTG5-27C)The posterior arcade is further away from the duodenum, so its vasa recta to the duodenum must be longer.
18a. Does the splenic vein receive the inferior mesenteric vein? (N311,N312,N313,TG5-14,TG5-28)The respective veins travel with the arteries of the duodenum and pancreas. They drain to the superior mesenteric vein and/or the portal vein.
19a. Do you find a lesser duodenal papilla? Are there differences between it and the greater duodenal papilla? (N279,TG5-26)Yes... well... sometimes. The splenic vein receives the inferior mesenteric vein in slightly more than a third of individuals, while inferior mesenteric vein first unites with superior mesenteric vein in approximately one third of individuals. In the remaining individuals (slightly less than a third), the three veins unite at the same point to form the portal vein.
20a. Into which part of the duodenum do the common bile and pancreatic ducts open? (N279,TG5-26)The lesser duodenal papilla can usually be found superior and anterior to the greater duodenal papilla. The accessory pancreatic duct opens here.
21a. Where is the inferior vena cava? (N287,N300,TG5-19)The descending (2nd) part of the duodenum.
22a. Do you have an accessory pancreatic duct? (N279,TG5-26)The inferior vena cava lies embedded within the posterior surface of the liver.
Do you? Most people do. The small accessory pancreatic duct drains the upper part of the head of the pancreas to the lesser duodenal papilla within the wall of the descending (2nd) part of the duodenum.